Total Nucleated Cell and Viable Cell Counts, a Complete guide: Introduction to Cell Counting
Total Nucleated Cell Count is a vital measurement in both research and clinical settings, especially in cord blood collection and bone marrow harvest procedures. It represents the total number of nucleated cells in a sample, including stem cells and immune cells, providing an essential snapshot of cellular content.
Accurate measurement of TNC helps in predicting engraftment success and assessing stem cell potency, ensuring effective transplantation and therapy outcomes.
Laboratories often rely on tools like flow cytometers and hematology analyzers to determine TNC, while careful sample handling and proper post-processing guarantee reliable results. Understanding TNC is the first step toward safe and effective stem cell therapy.
What is Total Nucleated Cell (TNC) Count?
The Total Nucleated Cell (TNC) count measures all nucleated cells in a sample, including white blood cells and stem cells. This number is a standard metric in umbilical cord blood, cord blood banking, and bone marrow harvest. By checking the median TNC count or using tools like a hematology analyzer or flow cytometer, labs can quickly determine if the sample meets transplantation requirements. Knowing factors affecting TNC concentration ensures the collected cells are both sufficient and functional.

Measuring TNC is essential for optimizing marrow collection volume and calculating marrow volume for TNC target. For instance, collecting too little marrow may not provide enough stem cells for the recipient, while excessive collection can lead to donor complications. By combining estimated collection volume and real-time measurements, clinicians can adjust procedures mid-operation. This approach helps in reducing donor procedure time and ensures the sample is safe and effective.
Understanding Cell Viability
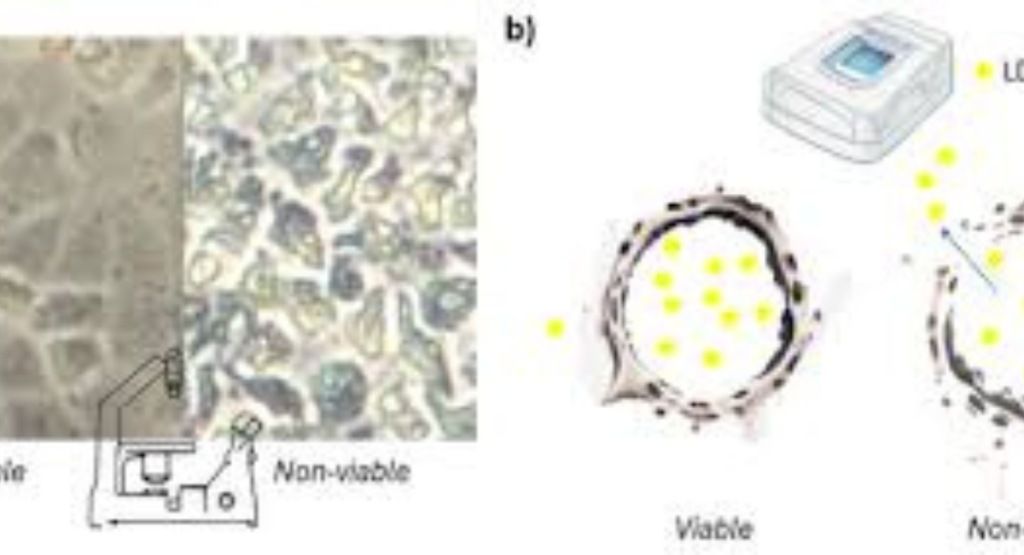
Cell viability indicates the proportion of living cells in a sample. Without viable cells, even a high TNC count is meaningless. Techniques like Trypan blue / Trypan purple dye and the 7-AAD viability test allow scientists to distinguish living cells from dead ones. Using these methods during post-processing stem cell measurement guarantees only healthy cells are used in therapy. Viability testing using 7-AAD is especially accurate and can be combined with CD34+ cell count analysis.
Maintaining high viability is critical for predicting engraftment success. Dead or damaged cells can reduce the cell recovery rate (%), impacting transplantation effectiveness. Labs also follow strict laboratory protocols for sample handling and filtration (removing fat, bone, clots). These practices protect both donor and recipient while improving overall stem cell functionality and potency.
CD34+ Cell Count Explained
The CD34+ cell count focuses on hematopoietic stem cells, a subset of the total nucleated cells. These stem cells are crucial because they can regenerate the patient’s blood and immune system. Measuring number of stem cells in cord blood helps in assessing cord blood potency and ensuring adequate TNC for transplantation. Using flow cytometry for stem cells is standard for detecting CD34+ cells.
Importance of CD34+ stem/progenitor cells cannot be overstated. They provide a reliable indication of stem cell functionality and engraftment prediction. A sample with high TNC but low CD34+ may not be effective. Combining CD34+ counts with TNC and viability data gives clinicians a complete picture, reducing the risk of treatment failure and improving patient outcomes.
Colony-Forming Unit (CFU) Assay
The Colony-Forming Unit (CFU) assay evaluates stem cell growth and function. In this method, cells are placed in a culture medium, allowed to grow, and counted after forming colonies. Measuring colony-forming units provides insight into stem cell potency beyond just numbers. It is a direct way of evaluating stem cell functionality in the lab.
CFU results complement TNC and CD34+ counts, giving clinicians a 360-degree view of the sample. While time-consuming, CFU is critical for predicting transplantation effectiveness. Different processing methods, like PrepaCyte-CB or Sepax, vary in CFU recovery, showing the importance of post-processing tests and careful sample handling.
Collection and Processing of Cells
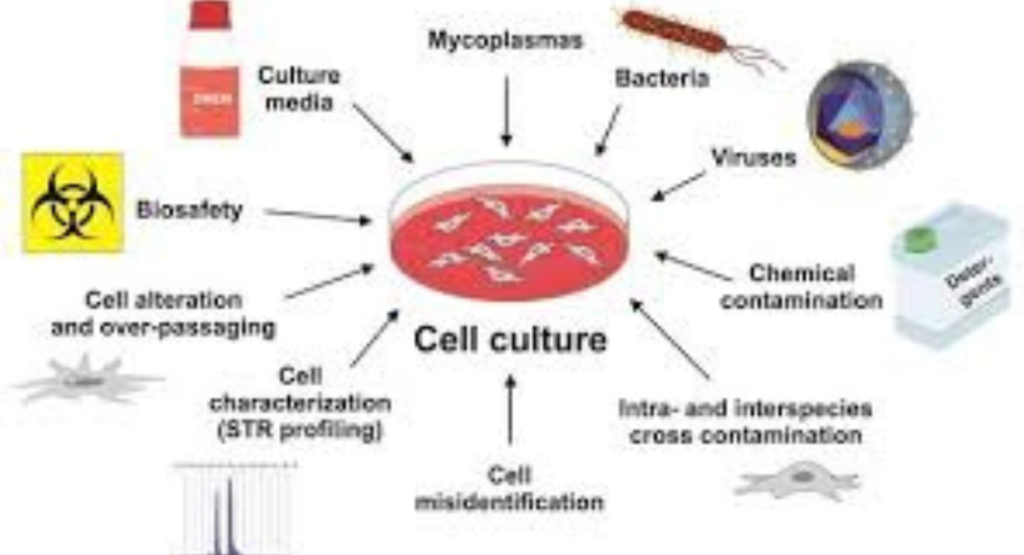
Cord blood collection and bone marrow collection are delicate procedures. The collection volume (mL) directly impacts TNC, CD34+, and CFU counts. Open collection kit or closed collection kit systems influence efficiency and risk of contamination. Filtering techniques like filtration (removing fat, bone, clots) ensure only usable cells remain.
After collection, labs perform post-processing stem cell measurement, using tools like flow cytometer and hematology analyzer for a complete blood count (CBC). These steps help in ensuring adequate TNC for transplantation and improving cell recovery rate (%). Proper handling reduces donor complications and maintains stem cell functionality.
Factors Affecting Accuracy of Cell Counts
Several elements can skew results. Sample handling, delayed processing, or poor mixing can reduce the accuracy of viable cell count and TNC measurements. Factors affecting TNC concentration include donor age, recipient body weight, and collection method. Even small errors in calculating marrow volume for TNC target can lead to under- or over-collection.
Lab instruments also matter. Using an automated hematology analyzer for TNC or flow cytometer requires proper calibration. Following laboratory protocols and monitoring post-viability percentage ensures accurate data. Ignoring these can affect predicting engraftment success and risk patient outcomes.
Improving Reliability of Counts
To improve reliability, repeat measurements and standardized methods are key. How to measure TNC concentration correctly involves real-time checks during bone marrow harvest. Standardization reduces variability and improves transplantation effectiveness. Training staff on viability testing using 7-AAD and determining viable cell count ensures consistent results.
Regular quality checks and post-processing tests can catch errors early. Monitoring relationship between collection volume and cell count allows clinicians to adjust protocols. This also minimizes donor complications and improves cell recovery rate (%), maintaining stem cell potency.
Applications in Research and Therapy
Total nucleated cell and viable cell counts have applications from lab research to clinical therapy. In cord blood banking, these metrics are crucial for assessing cord blood potency. In transplantation, accurate counts allow predicting engraftment success. Researchers also use counts to study hematopoietic stem cells and stem cell functionality.
In the USA, many hospitals and public cord blood banks rely on bone marrow collection data and cord blood collection statistics to guide clinical decisions. With proper sample handling, post-processing stem cell measurement, and accurate CD34+ cell count, clinicians can ensure high-quality treatment, reduce complications, and optimize patient recovery.
Conclusion and Key Takeaways
Understanding Total Nucleated Cell and Viable Cell Counts is fundamental for anyone involved in stem cell therapy. Accurate TNC, CD34+, CFU, and viability measurements ensure effective transplantation effectiveness and reduce risks for donors. Following proper laboratory protocols, sample handling, and post-processing tests guarantees safety and potency.
By combining these counts, clinicians and researchers can predict engraftment success, improve stem cell functionality, and ensure optimal outcomes. Whether in cord blood banking or bone marrow harvest, these measurements are the backbone of modern stem cell therapy in the USA.
Example Table: Key Metrics in Cell Counting
Metric Purpose Typical Range Tools/Methods
TNC Count Total nucleated cells 0.1–0.5 x10^8/mL Hematology analyzer, Flow cytometer
Viable Cell Count Live cells percentage >90% Trypan blue, 7-AAD test
CD34+ Count Stem/progenitor cells 1–2 million/mL Flow cytometry
CFU Assay Stem cell functionality Colony formation Culture media incubation
Meta Description
Learn how Total Nucleated Cell Count measures stem cells, predicts engraftment success, and ensures effective transplantation.
FAQs
What is a good total nucleated cell count?
A good total nucleated cell (TNC) count depends on the sample type, but in cord blood, higher counts generally indicate more stem cells and better transplant potential.
What does it mean when total nucleated cell count CSF is high?
A high TNC in cerebrospinal fluid (CSF) may indicate infection, inflammation, or bleeding in the central nervous system.
What if total cell count is high?
A high total cell count usually suggests infection, inflammation, or abnormal cell proliferation, depending on the sample source.
What is a normal total cell count?
Normal total cell counts vary by sample type; for blood, typical WBC counts range from 4,000–11,000 cells/µL, and CSF normally has 0–5 cells/µL.






