LEA Count: Understanding and Using Lymphocyte Esterase Activity in Medical Testing
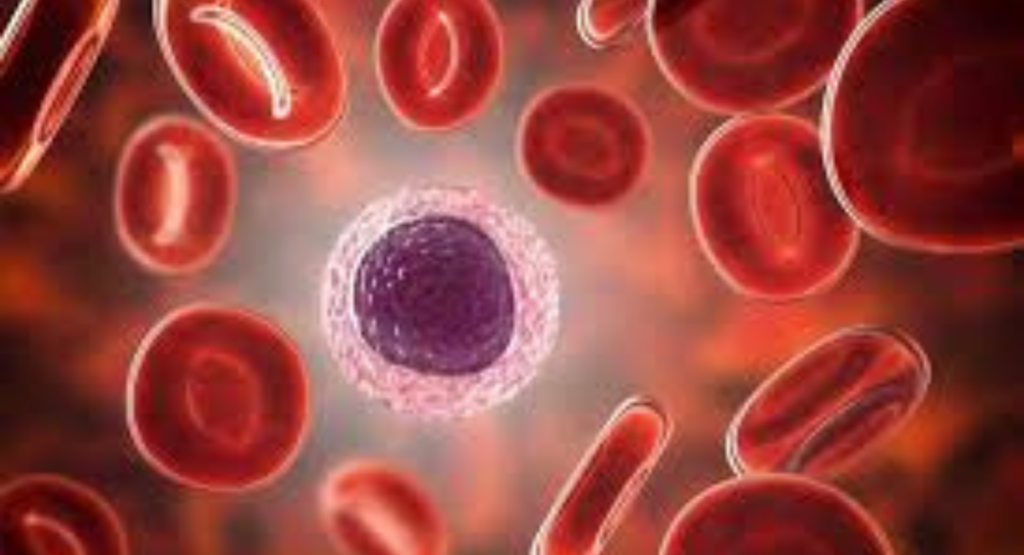
The LEA count is a crucial diagnostic tool that measures lymphocyte esterase activity, providing insights into white blood cells response in the body. Primarily used in urinalysis, it helps detect urinary tract infections (UTIs) and monitor inflammation, allowing healthcare providers to act quickly.
By assessing enzyme levels through simple urine tests or blood tests, clinicians can evaluate immune system activity and identify potential complications early. This non-invasive and cost-effective method supports routine laboratory testing in hospitals, clinics, and outpatient settings. Understanding LEA count results helps doctors make informed decisions, improve patient care, and track both acute infections and chronic conditions efficiently.
Clinical Importance of LEA Count
The LEA count plays a critical role in early infection detection. When white blood cells respond to bacteria, they release lymphocyte esterase, which can be detected in urine test or blood test samples. Elevated levels of LEA count indicate possible urinary tract infections (UTIs) or systemic inflammation. Clinicians use these results alongside symptoms to diagnose conditions quickly, which is essential for everyday computing of patient care data and timely decision-making.

Beyond UTIs, LEA count serves as a reliable inflammatory marker for immune system activity. It can help track chronic kidney disease progression or autoimmune flare-ups. Understanding these enzyme levels allows doctors to customize treatment plans and monitor patient recovery efficiently. Regular monitoring also provides insight into the immune system activity, helping predict potential complications before they worsen.
How LEA Count is Measured
Measurement of LEA count is typically done through urinalysis using either dipstick tests or automated analyzers. Dipstick tests change color when lymphocyte esterase activity is present, providing a quick visual indication. Automated devices quantify enzyme levels precisely, enabling healthcare professionals to track minor changes over time. This process ensures better accuracy for laboratory testing in clinics and hospitals.
Modern labs use a combination of enzyme assay techniques to measure LEA count more reliably. These instruments offer built-in function keys and user-friendly interfaces for smooth operation. They provide fast results, which is especially helpful during evening work or urgent casual work sessions in busy medical facilities. The integration of technology enhances both speed and accuracy in clinical decision-making.
Interpreting LEA Count Results
A normal LEA count usually indicates no active infection, while elevated levels suggest the presence of white blood cells responding to pathogens. Doctors consider other markers, such as leukocyte esterase, protein levels, and pH, to confirm a diagnosis. Reference ranges can differ depending on patient age, gender, and overall health status, requiring careful interpretation.
Interpreting LEA count also involves understanding the clinical context. For example, a slightly elevated enzyme level may not indicate serious illness in a healthy adult but could signal early infection in immunocompromised patients. Cross-referencing LEA count with other test results ensures precise infection detection and avoids unnecessary treatments.
Advantages of LEA Count Testing
One major advantage of LEA count testing is speed. Unlike bacterial cultures, which take 24–48 hours, urinalysis can provide near-instant results, allowing doctors to start treatment immediately. This is crucial for preventing complications in UTIs and other infections. Additionally, the test is non-invasive and inexpensive, making it suitable for regular monitoring.
Another benefit is its versatility in routine diagnostics. LEA count helps track both acute and chronic conditions, providing visual interest in patient charts through trends and data points. Its combination with automated analyzers ensures consistent results, supporting efficient workflow during long typing sessions in lab documentation.
Applications Beyond Urinary Tract Infections
While commonly associated with UTIs, LEA count has broader applications. It can help monitor autoimmune disorders, kidney disease, and other inflammatory conditions. Tracking lymphocyte esterase activity over time allows doctors to anticipate flare-ups and adjust treatment strategies proactively.

In research, LEA count provides insights into immune system activity for clinical studies, including oncology and immunotherapy. Scientists can correlate enzyme levels with treatment responses, improving patient care strategies. Its non-invasive nature makes it ideal for longitudinal studies without burdening participants.
Limitations and Considerations of LEA Count
Despite its usefulness, LEA count is not perfect. False positives may occur due to contamination or temporary inflammation, while diluted urine can produce false negatives. Clinicians must interpret results alongside patient symptoms and other laboratory tests.
Proper sample collection and handling are essential. Missteps can compromise enzyme assay results, leading to misdiagnosis. Therefore, LEA count should be one of several tools used to assess immune system activity, not the sole determinant for treatment decisions.
Technological Advances in LEA Count Testing
Recent innovations include automated urinalysis systems with integrated quality control, digital readings, and multi-marker analysis. Modern automated analyzers can simultaneously assess LEA count, nitrites, and protein, reducing errors and increasing efficiency.

These systems offer ease of navigation for lab technicians and improve workflow during high-volume testing. The combination of speed, precision, and reliability allows LEA count to play a central role in modern laboratory testing.
Conclusion: The Role of LEA Count in Modern Medicine
The LEA count is a critical tool for infection detection and monitoring immune system activity. Its speed, accuracy, and non-invasive nature make it essential in both routine and specialized diagnostics. Combining urinalysis, enzyme assay, and modern automated analyzers ensures healthcare providers can deliver timely, informed care.
From detecting UTIs to supporting chronic disease monitoring, LEA count has evolved into a versatile, indispensable component of contemporary medicine. By understanding and applying its results effectively, clinicians improve patient outcomes while maintaining a seamless workflow in busy medical environments.
Meta Description
Learn about LEA count, measuring lymphocyte esterase activity to detect infections, monitor inflammation, and track immune system health.
FAQs
What is LEA count?
LEA count measures lymphocyte esterase activity in urine or blood to detect infections and inflammation.
What is Lee Count?
“Lee Count” is likely a misspelling or misinterpretation of LEA count; it refers to the same enzyme test.
Is 60 LEA better than 80 LEA?
In fabrics, a higher LEA (yarn linear density) number means finer threads; 80 LEA is finer than 60 LEA.
What is the highest LEA in linen fabric?
High-quality linen can have LEA values up to 100–120, indicating very fine, smooth yarn.
Why does the Bible forbid wool and linen?
The Bible forbids mixing wool and linen (shatnez) as a symbolic separation of materials for ritual purity.
What is the unhealthiest fabric to wear?
Synthetic fabrics like polyester and nylon can trap heat and moisture, making them less breathable and potentially unhealthy.






